A Pediatric Emergency MD Sounds the Alarm on EpiPen Safety
I’ve recently spent some time connecting with Dr. Julie Brown, a Pediatric Emergency Medicine Physician and Associate Professor at the University of Washington. For the last several years, she has been sounding the alarm on injuries sustained after patients use the EpiPen. Her research is startling.
She uses social media to get the word out, both her Pinterest page and Facebook, but as she tried to bring awareness to larger organizations and platforms, her concerns were often met with silence.
Her story, in her own words, is below:
This is my story. I am a Pediatric Emergency Medicine Physician, working in a children’s hospital. While on shift one day, I received an ambulance delivering a 4-year-old boy who had suffered an anaphylactic reaction while at daycare. His daycare providers had appropriately decided to inject him with his EpiPen. Two of them together attempted to restrain him and hold the device in place for the required 10 seconds. He, not surprisingly, struggled, and the needle tore down his leg, resulting in a long leg laceration, and then dislodged. The daycare provider, believing it took the full 10 seconds to deliver the medication, instinctively tried to reinsert the needle, resulting in a second laceration. This poor young man thus not only required treatment for his anaphylaxis, he now also had two large wounds that required repair.
After this shift, I realized I didn’t know enough about EpiPens and how they worked. It seemed strange to me that such a small dose of epinephrine would take such a long time to eject from the device. And I couldn’t think of another situation in medicine where we would hold a needle in a child’s muscle for 10 seconds and expect that to happen without issue. So I decided to do a little investigating. First, I asked a colleague for a used EpiPen, which I fired off in a small light box I bought online, while videotaping. I ended up firing off many EpiPens, and you can watch one of these videos here: https://www.youtube.com/watch?v=r6ZkAx7djyk. What struck me was that the medication was always fully ejected in less than a second. Now I was even more puzzled. The more I researched, the more I realized there was little evidence to support holding the device for 10 seconds, and compelling evidence that 3 seconds was more than enough (I can share all this information in greater detail if you are interested). It seemed that the reason for the 10 second hold was historical, and related to the use of atropine injectors by the military as a nerve gas antidote. There were really no facts to support it as good practice for epinephrine devices. And yet, we were routinely subjecting parents and children to this 10-second hold.
Furthermore, I also discovered that nowhere in the instructions for use did it mention restraining a child while administering the medication, even in the pediatric formulations of the device, like EpiPen Jr. So these poor parents were being placed in a position of administering the device, holding a needle in their child’s thigh for 10 seconds, without even being given the simple advice to restrain their child. This seemed to me like an injury just waiting to happen. I thought I had better at least share with my colleagues what I had learned.
Here is where my journey really began. I emailed my colleagues and told them if they were prescribing an EpiPen, they should advise their caregivers to hold the child well, because I had cared for a child with leg lacerations, and the instructions for use said nothing about patient restraint. To my surprise, one of my colleagues replied that SHE had recently had a child with a leg laceration from an EpiPen. Now I knew I was on to something. I decided I had better explore the issue further. So I wrote an email and posted it on a Pediatric Emergency Medicine list-serve called PEM-L. And lo and behold, I heard about another 11 cases, plus a few other injuries. And what’s more, one of the physicians said the mother of his patient told her that she had seen photos of similar injuries on a Facebook allergy group called No Nuts Moms.
What happened next changed me and my career forever. I naively joined the closed group ‘No Nuts Moms’ to ask about leg lacerations from EpiPens. And I learned about many more, from some of the most amazing allergy moms I could ever hope to know, who selflessly shared their stories of the most traumatic days of their lives. But they and other allergy parents also opened my eyes to how much more I needed to understand about food allergies and anaphylaxis, the poor state of anaphylaxis care across the country, and the need for more research and education in the area of emergency care. I heard stories that literally made me feel ill, of children being placed at terrible risk by providers who knew less about anaphylaxis than the patient’s parents. These parents have educated me, and asked fantastic questions that have led me down paths of inquiry, so that I in turn could educate them. I have since made dozens of YouTube videos, and have Pinterest pages specific to auto-injectors, based largely on work I have done dissecting and examining these devices: https://www.pinterest.com/Donteatmagnets/epinephrine-auto-injectors-eais-epipen-auvi-qtm-al/. My understanding of these devices has been driven by the questions of these allergy moms, and I couldn’t have produced anything like the same quality of educational materials or research without the give-and-take relationship that two years of almost daily interacting on this Facebook group allowed. I am now considered an honorary allergy mom, a title I wear proudly. I am committed to focusing on anaphylaxis research for the rest of my medical career, which makes me fairly unique amongst emergency medicine colleagues. But emergency providers are needed in this field, as they are the ones who are responsible for providing the first response in the event of allergic reactions, and need the training and tools do that job well.
Ultimately, we ended up to with 26 cases of EpiPen-associated injuries, which we published, along with a review of the literature supporting a rapid release of epinephrine from the Epipen device, and recommendations for reducing the Epipen hold time. We also recommended adding restraint recommendations to the patient instructions for all epinephrine devices. A succinct summary of our research can be seen here: https://www.aaaai.org/global/latest-research-summaries/New-Research-from-JACI-In-Practice/epinephrine-autoinjectors-(1) and the full original article (which is quite graphic) is here: http://www.annemergmed.com/article/S0196-0644(15)00588-0/fulltext.
Two FDA officers, one in charge of safety and one in charge of labeling, recently emailed me to say that it was our research that was the primary driving force behind recent FDA changes, which include reducing the EpiPen hold time to 3 seconds, and adding restraint instructions to all auto-injector patient instruction materials: http://www.accessdata.fda.gov/drugsatfda_docs/label/2016/019430s061lbl.pdf#Patient. I am proud that our research was instrumental in making this change, and in making the use of EpiPens and other auto-injectors safer for children.
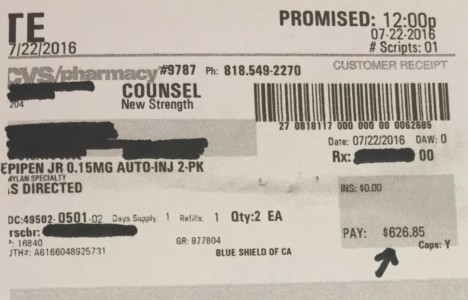
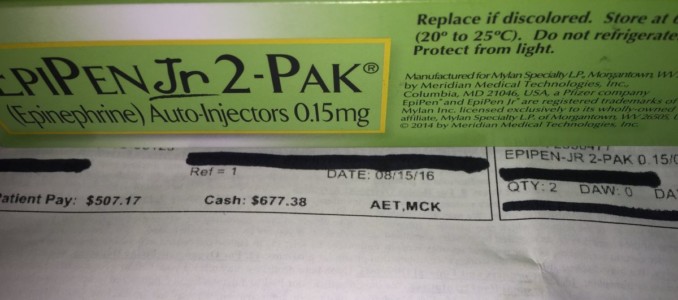
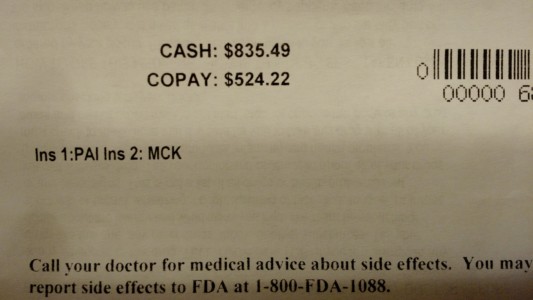
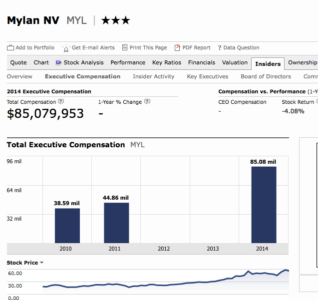
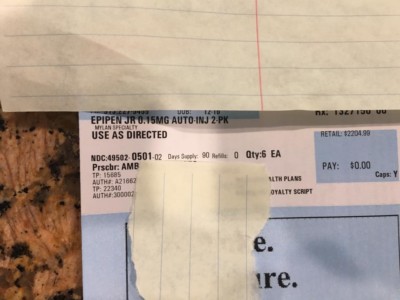
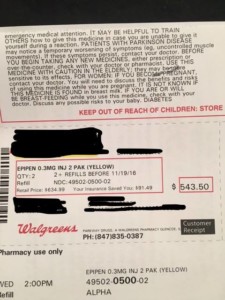
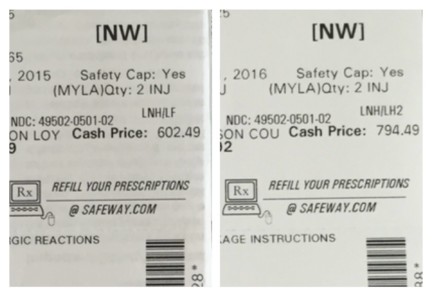
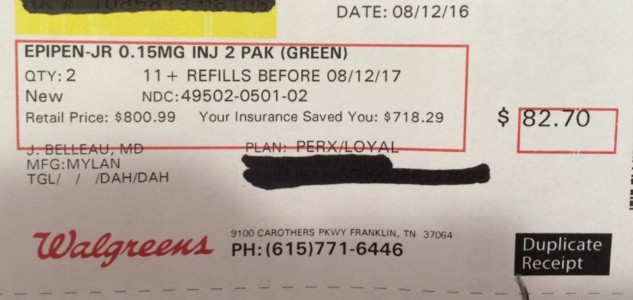
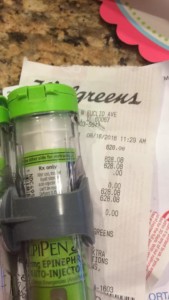
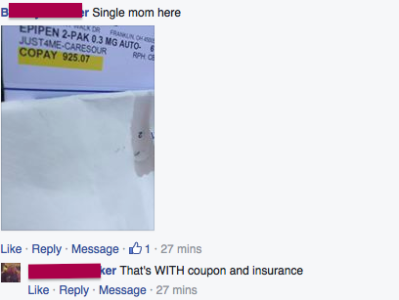
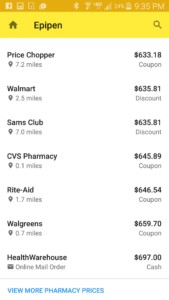
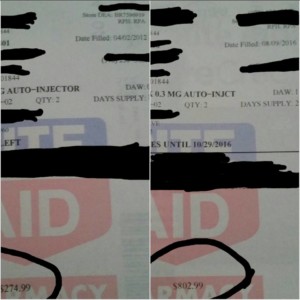
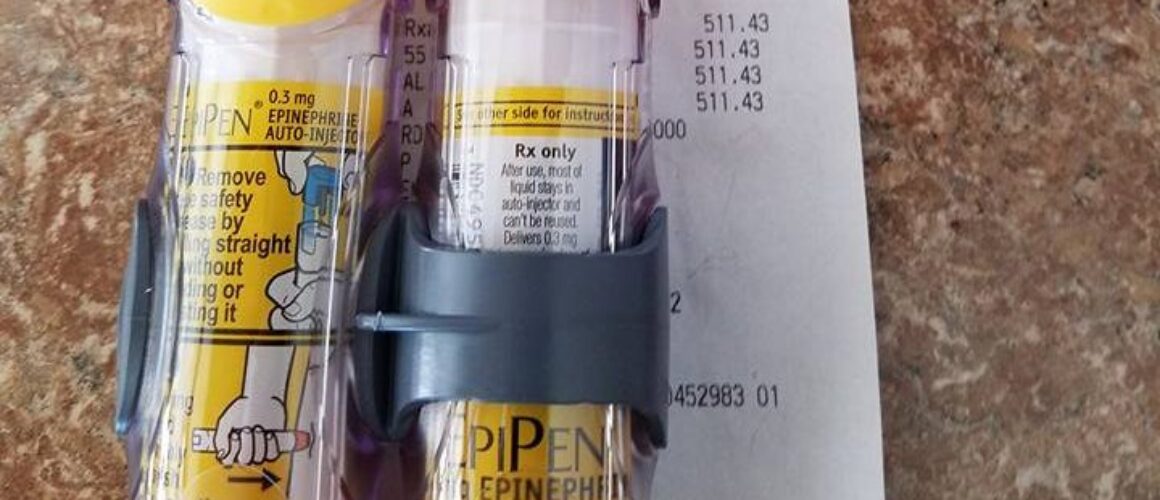
This study, and these FDA changes, are only the beginning for me. Driven by a passion to improve the lives of people with food allergies, and fueled by the many unanswered questions that have stacked up over the past two years, I have many other projects in progress. Our current work involves understanding the challenges around auto-injector use, and emergency preparedness. We recently published a systematic review of epinephrine stability at extreme temperatures, which is a first step in working towards expanding allowed temperature ranges for auto-injectors. We are also nearing completion of a systematic review of the stability of epinephrine when drawn up into a syringe. While this is never a good solution for anyone, the reality is that some patients are currently going without ANY epinephrine due to the high costs of auto-injectors, so a better understanding of the alternatives is important. It is also relevant to emergency care, where syringes and ampules are often used, and can result in delays to care while doses are calculated and drawn up.
In the future, I hope to do pharmacokinetic research—evaluating epinephrine levels in children in anaphylaxis, which has never been done (even in adults). I also have many ideas for education and research to improve emergency anaphylaxis care, including an anaphylaxis rap that I wrote and am trying to figure out how to get produced.
The largest barrier to accomplishing all these research goals is funding. I am frustrated by the time wasted trying to secure dwindling sources of funding that could be spent doing the research and improving the lives of children with allergies. I have a fundraising site: http://giveto.seattlechildrens.org/anaphylaxis. Please help if you can.
Please consider supporting the work of Dr. Julie Brown. She is a brave voice in our efforts to protect those with life threatening allergies.
You can reach her funding page here http://giveto.seattlechildrens.org/anaphylaxis
Facebook page: https://www.facebook.com/profile.php?id=1563285626
Twitter: @donteatmagnets
And the pinterest page. https://www.pinterest.com/Donteatmagnets/