Food Allergies & Food Sensitivities: Know the Signs, Know the Difference
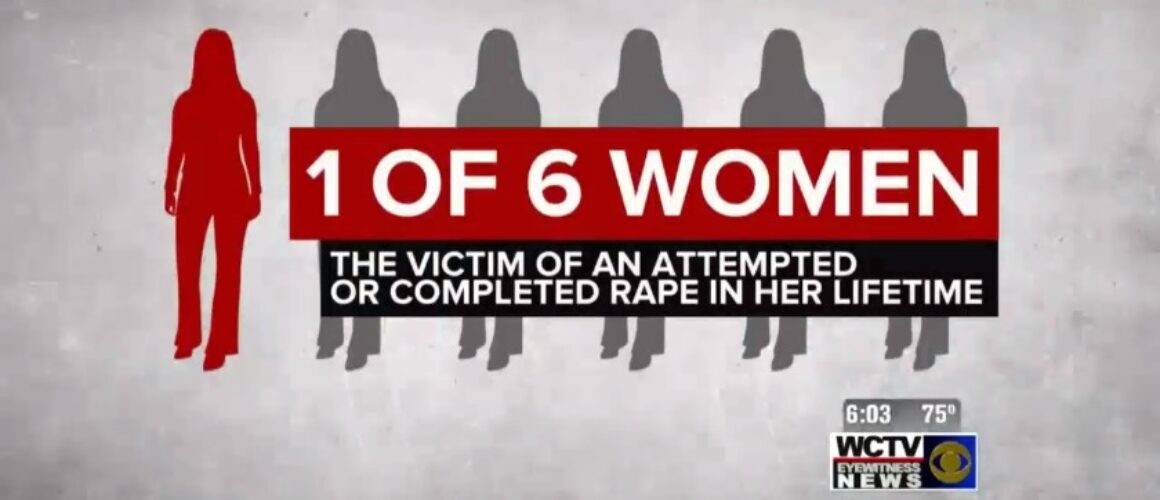
A life threatening allergic reaction to food sends someone to the emergency room in the United States once every three minutes. On November 24th, 2016, it was Oakley Debbs. He’d visited the ER multiple times for his asthma, but it was his nut allergy that sent him there where he died in his dad’s arms last year at the age of 11.
Too many of us are unfamiliar with the symptoms and signs of an allergic reaction until it happens to us or to one of our children. We can not repeat this information enough. We’ve had so many families say, “If I’d only known….”
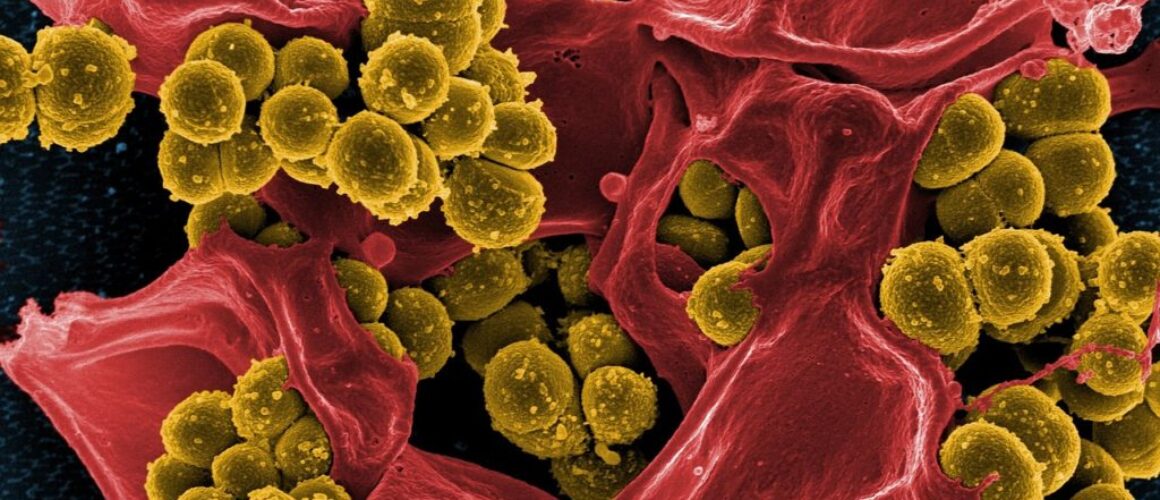
Today, one in ten children struggle with asthma, and one in four are affected by allergies. The incidence of allergy has increased significantly over the past two decades, and allergy to peanuts has more than quadrupled from 1997 to 2010. Approximately 30 million children – more than 1/3 of our kids – are affected by one of these four new childhood epidemics. This is not something we can just accept.
More importantly, the deaths have to stop. The most important thing is to know the symptoms, understand the condition and always be ready to administer epinephrine.
An official statistic held that allergies affect some 7 million Americans, including about 6 percent of children below the age of three. That information came courtesy of U.S. Food and Drug Administration Deputy Commissioner Lester M. Crawford, J., D.V.M., Ph.D., speaking before the Consumer Federation of America on April 22, 2002. But that data is now over ten years old.

The Centers for Disease Control issued a report in 2008 that said that there has been a 265% increase in the rate of hospitalizations related to food allergic reactions over the prior ten year period. Epipen, which has secured a monopoly in the space with over 90% market share, is now a $1.3 billion brand.
This begs explanation
An allergy is basically an overreaction by your immune system to a protein that it perceives as a threat—for example, the proteins in particular types of food, the dust mite protein, or pollen. For people without allergies, these proteins are harmless. But if you’ve got an allergy, your immune system sees these proteins as dangerous invaders.
To drive the invader out, your immune system mobilizes all its resources: mucous, to flush out the intruder; vomiting, to force it out; diarrhea, to expel it quickly. Such conditions may make you feel sick, but they’re actually evidence of your body’s attempts to get well.
A key aspect of the immune response is known as inflammation, characterized by one or more of four classic symptoms: redness, heat, swelling, and pain. Inflammation doesn’t occur only in allergic reactions; it flares up whenever your body feels threatened, in response to a bruise, cut, bacteria, or virus as well as to otherwise harmless pollen, dust, or food. Scientists now believe that much of our immune system is found in our digestive tracts, where many of these inflammatory reactions occur in the form of stomachaches, cramping, nausea, bloating, and vomiting.
Ironically, the immune system’s inflammatory reaction—meant to heal and protect the body—often causes more problems than the initial “invader” in the cases when allergic reactions become life-threatening.
Common Symptoms of Food Allergy: Immediate Reactions
- rash or hives
- nausea
- vomiting
- stomach pain
- diarrhea
- itchy skin
- eczema
- shortness of breath
- chest pain
- swelling of the airways to the lungs
- anaphylaxis
Food Allergies and Food Sensitivity: Our Immune System Overreacts Again
At first glance, the distinction between “allergies” and “sensitivity” may seem like a meaningless word game. But understanding the relationship between these two conditions is crucial to grasping the true nature of the allergy epidemic—and to seeing how even the supposedly healthy foods in our kitchens may be harmful to our health.
As we’ve seen, allergies are an overreaction of our immune system, a kind of exaggerated response to a perceived danger. When a child comes in contact with these proteins (peanut, egg, wheat, etc.) her immune system “recognizes” the protein as dangerous, just as it would have seen the danger in the bacterium that causes pneumonia or the virus that causes mumps. In response, her immune system creates special “fighter” proteins called antibodies designed to identify and neutralize the “invader.”
These fighter proteins are known as immunoglobulin E, or IgE for short. When they’re released into the bloodstream, their purpose is to “seek and destroy” the invader, which they do by creating one or more of the classic food allergy symptoms, such as the hives, or the diarrhea with which other children respond, or, in more extreme cases, the anaphylactic shock that can kill a child within minutes.
The classic IgE response occurs within minutes or even seconds, because IgE proteins are some of the most aggressive antibodies we know. That immediate IgE response is the defining characteristic of an allergic reaction.
Food sensitivities start out in a similar way. If a “sensitive” child is exposed to a protein that his system perceives as a threat, he’ll manufacture another type of fighter protein, known as Immunglobulin G, or IgG. Although IgE and IgG antibodies play similar roles, they produce somewhat different—though often overlapping—symptoms.
A crucial difference between the two, though, is their reaction time. The less aggressive IgG antibodies typically produce a delayed response that might not appear for hours or even days after the child has consumed the offending food.
So even though food sensitivities and food allergies both produce painful, inflammatory, and potentially dangerous responses, this delayed reaction time has led many doctors to give food sensitivities second-class status. Partly that’s because they don’t present an immediate and obvious threat to children’s lives: only the IgE proteins trigger anaphylactic shock, for example, and in that sense, only the IgE proteins can kill (though the IgG reaction can have serious long-term consequences). I also think that traditional doctors tend to downplay the importance of nutrition, frequently dismissing the idea that such symptoms as earache, eczema, crankiness, brain fog, and sleep problems might be related to a child’s diet.
However, an article in The Lancet, Britain’s most respected medical journal, casts another light on the subject. The article referred to doctors who use elimination diets—diets that begin with a very limited, “safe” array of food choices and then add potentially problematic foods back into the diet, one by one.
When you take a break from eating that problem food, however, and then add it back into your diet, you see how powerful its effects are and how responsible it may be for a seemingly unrelated problem. Foods that you thought were safe for you turn out to be highly problematic, indicating the presence of a previous undiagnosed food sensitivity. As a result, the authors of the Lancet article conclude that the prevalence of food sensitivity (referred to in the article as “food intolerance”) has been seriously underestimated.
Certainly, food allergies are far more dramatic. Whenever you read about a kid who died within minutes of eating at a fast-food joint or after breathing in the peanut dust from a friend’s candy wrapper, that’s an “IgE-mediated” food allergy. They’re fast, they can be deadly.
But doctors should be looking at delayed reactions, too, the “IgG-mediated” responses to food sensitivities. And some doctors do look seriously at both. Most conventional doctors, though, tend to focus on IgE immediate reactions. I think there are lots of reasons why they should view the two types of reactions as part of a larger, single problem.
First, both reactions have the same ultimate cause: the immune system’s overreaction to apparently harmless food. According to internationally acclaimed author and physician Kenneth Bock, M.D., there’s also quite a bit of overlap between IgE and IgG symptoms. Both can contribute to inflammatory responses in multiple body systems.
True, the delayed IgG reactions are less likely to cause hives and are more likely to produce a host of apparently vague symptoms, such as headache, brain fog, sleep problems, joint pain, fatigue, and muscle aches. But both the immediate and the delayed responses are immune system problems triggered by a supposedly “harmless” food.
Conventional doctors’ tendency to separate “IgE-mediated” food allergies and “IgG-mediated” food sensitivities into two separate problems has the effect of minimizing the allergy epidemic. Remember, IgE allergies, IgG sensitivities, and asthma—three similar ways that our immune systems can overreact—are all on the rise. It makes sense to find a doctor who is willing to address all three as symptoms of a greater underlying issue.
Common Symptoms of Food Sensitivity: Delayed Reactions
- fatigue
- gastrointestinal problems, including bloating and gas
- itchy skin and skin rashes like eczema
- brain fog
- muscle or joint aches
- headache
- sleeplessness and sleep disorders
- chronic rhinitis (runny nose), congestion, and post-nasal drip
Five Take-Aways:
1. Even if your kids can’t talk, their skin speaks volumes! Did you know that the skin is a person’s largest organ? Even when your kid is too young to tell you how he feels or too used to her symptoms to identify them (when kids hurt all the time, they don’t know they hurt!), you can often read your child’s condition in his or her skin.
Does your kid have eczema? Does he get rashes around the mouth, especially after he eats a certain food or swallows a certain beverage? Rashes around the knees, elbows, or armpits? Does he have “allergic shiners”—that is, dark circles under the eyes?
These are all inflammatory reactions, signs that the body is trying to rid itself of what it perceives as “toxic invader.” In your child’s case, that “toxic invader” might be an apparently harmless food, to which your kid is either allergic or “sensitive.” Keeping that invader away from your kid may bring relief from symptoms—and it may clear up other problems, such as brain fog, crankiness, sleep problems, inattention, acne, and mood swings.
2. Look below. Your kids’ bowel movements, not to be too delicate here, also speak volumes. Runny poops are a sign that a person isn’t properly digesting his food. And indeed, as we got the allergens out of some children’s diets, poops tend to firm up.
3. Chronic ear infections are often a sign of dairy allergies. In some cases, milk may have ill effects like eczema, upset stomachs or chronic ear infections for children who are allergic or sensitive to it.
4. Find a doctor who is willing to work with you, test for both IgE and IgG allergies and sensitivities and to address the important role that elimination diets can play in managing allergic symptoms like eczema, ear infections and chronic mucous.
5. More research is needed. Food allergies are impacting a growing number of Americans. It is impacting everything from how schools feed children to what snacks airlines choose to carry on planes. Napster co-founder, Sean Parker, recently donated $24 million to Stanford to conduct research to get to the bottom of this condition, what is triggering it and how to cure it.
6. Find a friend. Find an ally to help you get safe snacks in the classroom or meet with your Congressman to discuss this epidemic. The landscape of childhood is changing. It is changing families and changing the food industry. None of us can do everything, but all of us can do something.
Always discuss individual health inquiries and medical issues with a qualified personal physician and/or specialist.
In honor of Oakley, many of us changed our profile picture on Facebook and across social media in memory of Oakley. Please don’t hesitate to join us and use the image below.