U.S. of Allergies: How EpiPen Became a Billion-Dollar Brand
 The number of people in the U.S. with food allergies is skyrocketing.
The number of people in the U.S. with food allergies is skyrocketing.
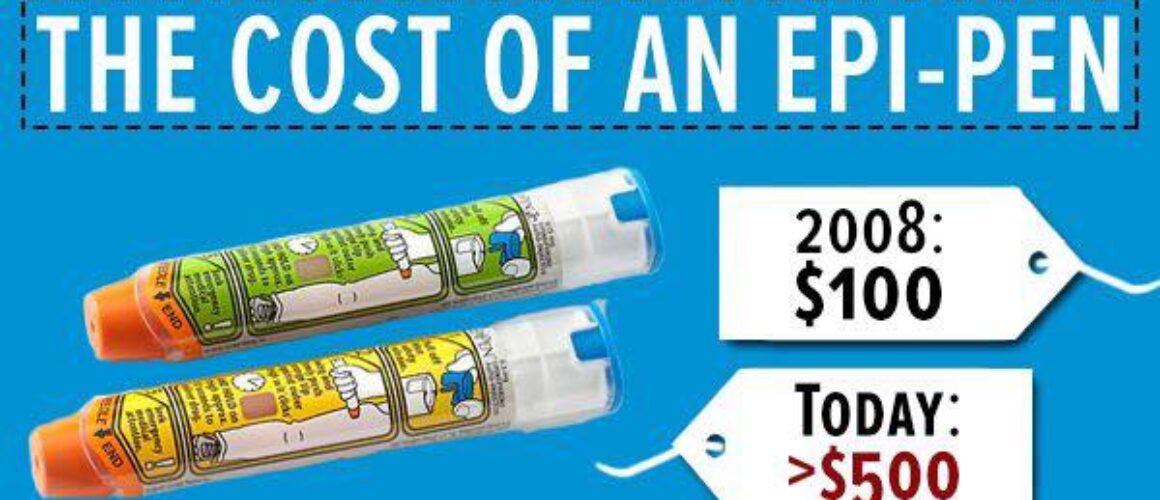
For the last year, we’ve been working to bring an awareness to the risk that the skyrocketing price of EpiPens creates, and the fact that some families are now priced out of this life saving devices due to its jaw-dropping price tag of about $600.
As recently as the 3rd quarter of 2015, the price of one EpiPen was at $300. But that number is misleading, as the product is sold in a two-pack, so the consumer has to pay $600. In some cases, like this week in Colorado, a parent paid over $700 for the exact same device that just six years ago cost $100. No product changes, no device changes, and the key ingredient inside only costs a few dollars.
So what’s going on?
There is very little competition on the market which only makes matters worse. Last year, Auvi-Q, an alternative device designed by twin brothers who wanted an easy-to-carry option was recalled. The New York Times covered their amazing story in 2013 and the sale of their company to Sanofi. It was short-lived.
According to the FDA, “As of October 26, 2015, Sanofi has received 26 reports of suspected device malfunctions in the US and Canada. None of these device malfunction reports have been confirmed.”
So the entire product line was recalled because of 26 unconfirmed reports. 26 unconfirmed reports.
Apparently, a very similar device is also used to deliver other medications and no reports have been mentioned or product recalls announced. According to Kaleo Pharma, “on April 3, 2014, the FDA approved EVZIO, the first and only naloxone auto-injector intended to be available for emergency administration by family members or caregivers in cases of known or suspected opioid overdose. The company’s first product approval, Auvi-Q™ (www.Auvi-Q.com) (Allerject™ in Canada), was licensed to Sanofi US which launched the product in early 2013.”
Kaléo, the developer of the Auvi-Q epinephrine auto-injector appears to be planning the return of its “talking” device to market.
The Virginia-based company recently regained the rights to the auto-injector from Sanofi US following a full device recall in the fall of 2015. “We now own the product. We are in the process of figuring out when and how best to bring Auvi-Q back to the market,” Spencer Williamson, president and CEO of Kaléo. According to the Richmond Times “earlier this year, Sanofi US and Kaléo terminated a 2009 agreement that called for Sanofi to manufacture and market the Auvi-Q auto injector.
“A Sanofi representative at the time said the company was able to retrieve some of the 26 devices consumers reported not working correctly but was not able to identify a malfunction in the device.”
The entire product line was recalled because of 26 unconfirmed reports that the company itself was not able to identify.

The rate of people with peanut allergy in the United States more than quadrupled between 1997 and 2010. A life-threatening food allergic reaction now sends someone to the E.R. once every three minutes in the U.S.
The food industry is getting in on it. Mondelez, formerly known as Kraft, recently acquired Enjoy Life Foods, a popular and well-loved brand in the allergy space, free from many of the top eight allergens and also free from genetically modified ingredients.
It was a $40 million company that was acquired for over $80 million.
What does Mondelez plan to do with the acquisition? Grow it into a billion dollar brand.
What are some other billion dollar brands? Cheerios, Lays, Pepsi, Starbucks….
And EpiPen.
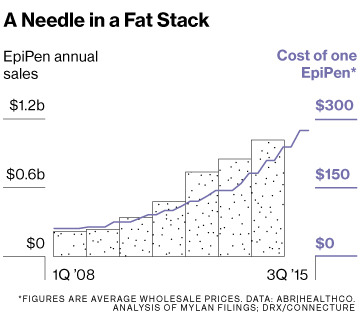
According to Bloomberg, “In a 2007 purchase of medicines from Merck, drug maker Mylan picked up a decades-old product, the EpiPen auto injector for food allergy and bee-sting emergencies. Management first thought to divest the aging device, which logged only $200 million in revenue. Today, it’s a $1.2 billion-a-year product that clobbers its rivals and provides about 40 percent of Mylan’s operating profits.”
Food allergies are not a niche, it is a growing epidemic that is challenging how we think about our food and how it is made. Genetic factors don’t change this quickly, environmental factors do. Are we allergic to food or to what’s been done to it? A lot of families now pay more for free-from food, because we don’t know the answer to that question.
Researchers reporting in the Journal of the American Medical Association states that the costs of food allergies, from medical care to food to pharmaceuticals is $4,184 per child per year, costing our economy $25 billion, including lost productivity.
On top of that, the costs to families with food allergies is skyrocketing. After insurance company discounts, a package of two EpiPens costs about $415. By comparison, in France, where Meda sells the drug, two EpiPens cost about $85. Back in 2007, when the company was purchased, it cost $57. EpiPens wholesale price rose 400% since 2007 and 32% in the last year alone. EpiPen margins were 55 percent in 2014, up from 9 percent in 2008.
To discount this condition in any way is irresponsible, but it is just one of the conditions that is triggering a food awakening around the country.
In the last year, Target, Chipotle, Kroger, even General Mills and Cheerios have responded to this growing demand in the marketplace. Free-from foods are showing up in Dollar Tree stores.
These companies aren’t stupid. They see the escalating rates of diseases in their own employees, they feel the financial impact with their own health care costs, and they hear consumers that are saying they want to eat fewer fake, artificial and genetically engineered ingredients.
While the chemical companies selling these new ingredients say there is no evidence of harm, consumers are saying: there is no evidence since these ingredients were never labeled in the United States.
In other words, if you walked into an allergist’s office and asked if you were allergic to soy that has been in the food supply for thousands of years or if you are allergic to Roundup Ready soy, non-GMO soy treated with Roundup or organic soy, there would be no test to give you that answer. Next time, you are at the allergist’s office, ask which soy they are testing for.

A study released in the Journal of the American Medical Association, says yes, living in the United States increases your risk of allergic diseases……“significantly.”
“Living in the US raises risk of allergies,” says the headline.
According to the research, living in the United States for a decade or more may raise the risk of some allergies, reports the Journal of the American Medical Association.
“These data indicate that duration of residence in the United States is a previously unrecognized factor in the epidemiology of atopic disease,” it said.
In other words, the longer you live here, the more likely you are to develop some kind of allergy, asthma, eczema or other related condition.
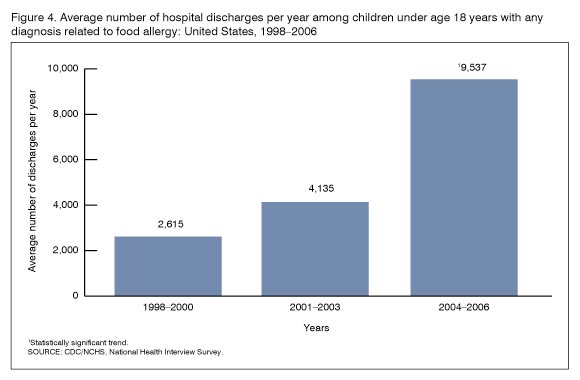
Food allergies have been skyrocketing in the United States in the last fifteen years. Not only has the CDC reported a 265% increase in the rates of hospitalizations related to food allergic reactions in a ten year period, but the sales of EpiPens, a life-saving medical device for those with food allergies, has also seen record sales growth according to the New York Times.
So what’s going on?
The study aimed to find out. Allergies reported in the survey included asthma, eczema, hay fever, and food allergies.
“Children born outside the United States had significantly lower prevalence of any allergic diseases (20.3%) than those born in the United States (34.5%),” said the study led by Jonathan Silverberg of St. Luke’s-Roosevelt Hospital Center in New York.
Let’s restate that:
Children born in the US have more than a 1 in 3 chance of having allergic diseases like food allergies, asthma or eczema, while kids born in other countries around the world had a “significantly lower prevalence” of 1 in 5.
On top of that, “foreign-born Americans develop increased risk for allergic disease with prolonged residence in the United States,” it said.
In other words, if you move here, your chances of developing any one or more of these allergic diseases increase.
The study went so far as to say that children born outside of the US who moved here showed “significantly” higher odds of developing these diseases.
What’s driving this? Is it really Purel and intense handwashing? And the hygiene hypothesis?
And are we allergic to food? Or what’s been done to it?
Because genetics don’t change that quickly, and the environment does.
This presents a risk not only to these children, but also to our economy, as the financial burden of these conditions and their associated health care costs impact not only families but also our country, our military and our productivity.
So what is triggering this escalating, US allergy epidemic?
According to Reuters report on the study and Dr. Ruchi Gupta, who studies allergies at the Northwestern University Feinberg School of Medicine in Chicago but wasn’t involved in the new research, “This is definitely something we see clinically and we’re trying to better understand, what is it in our environment that’s increasing the risk of allergic disease?” said
“Food allergies have increased tremendously,” she told Reuters Health. “We do see people who come from other countries don’t tend to have it.”
According to Science Daily:
Genetically engineered crops are created by inserting a protein from a different organism into the original crop’s genome. This is usually done to create a plant that is more resistant to insects or diseases.
The Food and Agriculture Organization within the World Health Organization has a structured approach to determining whether genetically engineered foods cause allergies, according to Venu Gangur, MSU assistant professor of food science and human nutrition, who also is a faculty member in the National Food Safety and Toxicology Center. “But it has a major flaw. A critical question in that process asks, ‘Does the protein cause an allergic reaction in animals?’ The problem is that there has been no good animal model available to test this.”
It’s food for thought.
The cost of food allergies is burdening more than just the families dealing with them, it’s burdening our schools, our health care system and our economy. It has become a billion dollar business in less than a decade for the company making EpiPens, so they have no reason to stop it.
Until there’s a cure, there’s EpiPen, but there used to be TwinJect and Auvi-Q, too. They are both gone, and consumers are left with a product on the market that was first originally used by the military, whose patent somehow hasn’t expired and whose design has invited countless criticism from both patients and practitioners for its broken needles. It leaves a lot to be desired and a lot of Americans asking the one question: Why 6 price increases in 6 years for a now $600 device?
It reminds us here of another company and their infamous tagline: Ask Why.
That company was Enron. And it’s time for both consumers and members of Congress to “ask why” we are seeing this outrageous increase in the price of EpiPens.
Lives are at risk.